Welcome to our article on stem cell approaches for sickle cell anemia treatment. Sickle cell disease (SCD) affects thousands of Americans and millions worldwide, primarily those of African descent. Unfortunately, it remains an incurable condition for most individuals. However, there is hope in the form of stem cell strategies that offer the potential for a cure.
Stem cell transplantation, specifically hematopoietic stem cell transplantation (HSCT), has emerged as a curative option for sickle cell disease. HSCT can be performed using the patient’s own genetically modified stem cells (autologous) or stem cells from a suitable donor (allogeneic). While HSCT comes with significant risks and complications, it remains the only available curative therapy for SCD.
Key Takeaways:
- Hematopoietic stem cell transplantation (HSCT) is a potential cure for sickle cell disease.
- HSCT can be autologous or allogeneic, using the patient’s own modified stem cells or those from a suitable donor.
- HSCT is associated with significant risks and complications, but it offers hope for a cure.
- SCD mainly affects individuals of African descent, with limited treatment options available.
- Stem cell strategies provide a promising avenue for improving the lives of those living with sickle cell disease.
Understanding Sickle Cell Disease
Sickle cell disease is a genetic blood disorder characterized by mutations in the beta-globin gene, leading to the production of abnormal hemoglobin. This abnormal hemoglobin causes red blood cells to become rigid and adopt a sickle-like shape when exposed to a low-oxygen environment.
As a result, these deformed red blood cells have difficulty flowing smoothly through blood vessels, leading to blockages and reduced oxygen supply. This can cause severe pain, organ damage, and a range of complications throughout the body.
It is estimated that sickle cell disease affects approximately 100,000 people in the United States, primarily individuals of African descent. However, it can occur in individuals from other ethnic backgrounds as well.
The primary genetic defect responsible for sickle cell disease is a point mutation in the beta-globin gene that leads to the substitution of a single amino acid in the hemoglobin protein. This mutation results in the production of an abnormal form of hemoglobin known as hemoglobin S.
“Sickle cell disease results in multiple organ damage due to blocked blood vessels and organ ischemia.”
Hematopoietic Stem Cell Transplantation (HSCT) for SCD
Hematopoietic stem cell transplantation (HSCT) is a curative option for individuals with sickle cell disease (SCD). HSCT can be either autologous, which involves genetic modification of the patient’s own stem cells, or allogeneic, where stem cells from a suitable donor are used. This procedure offers hope for patients with severe SCD and complications such as stroke, acute chest syndrome, recurrent pain crises, nephropathy, and retinopathy.
However, the decision to proceed with HSCT is complex and requires careful consideration of the potential benefits and risks. Suitable donors, especially fully matched siblings, greatly increase the chances of a successful transplant.
| Indications for HSCT |
|---|
| Severe sickle cell disease |
| Complications such as stroke |
| Acute chest syndrome |
| Recurrent pain crises |
| Nephropathy |
| Retinopathy |
HSCT remains the only available curative therapy for sickle cell disease, providing the potential for long-term remission and improved quality of life. Ongoing research and advancements in stem cell transplantation techniques continue to refine the procedure, making it a promising option for individuals with SCD.
Gene Therapy for Sickle Cell Disease
In recent years, gene therapy has emerged as a promising approach for the treatment of sickle cell disease. One particularly promising gene therapy technique is LentiGlobin. Through LentiGlobin gene therapy, blood-forming stem cells are collected from the patient’s body. These stem cells are then modified by introducing a corrected version of the beta-globin gene using lentiviruses. The modified stem cells are reinfused into the patient’s bone marrow, where they begin producing healthy red blood cells. This innovative approach has the potential to eliminate episodes of severe pain associated with sickle cell crisis and improve the morphology of red blood cells.
Clinical trials utilizing gene therapy, such as LentiGlobin, have demonstrated promising long-term outcomes in the elimination of severe pain crises in individuals with sickle cell disease [Second source]. This groundbreaking research offers hope for individuals living with this debilitating condition, providing the potential for a life free from the limitations imposed by sickle cell crisis.
Advantages of Gene Therapy for Sickle Cell Disease
Gene therapy, such as LentiGlobin, offers several advantages over traditional treatment methods for sickle cell disease:
- Elimination of severe pain crises: Gene therapy has the potential to eliminate episodes of severe pain associated with sickle cell crisis, improving the quality of life for individuals living with the disease.
- Improvement in red blood cell shape: Through gene therapy, the production of healthy red blood cells can improve the shape and function of these cells, reducing the occurrence of complications resulting from their abnormal morphology.
- Curative potential: With successful implementation, gene therapy has the ability to provide a long-term, possibly curative option for sickle cell disease.
Challenges and Future Directions
While gene therapy holds significant promise for the treatment of sickle cell disease, several challenges remain. The accessibility and affordability of gene therapies like LentiGlobin pose barriers to widespread implementation. Additionally, the long-term safety and durability of gene therapy outcomes require further investigation.
However, ongoing research and advancements in the field continue to address these challenges. Ongoing clinical trials and initiatives, such as the Cure Sickle Cell Initiative, aim to further develop and refine gene therapy approaches for sickle cell disease [First source, Second source]. As the field progresses, it is anticipated that gene therapy will play a crucial role in the future of sickle cell disease treatment, offering hope to millions of individuals affected by this condition.
Comparison of Gene Therapy and Traditional Treatments for Sickle Cell Disease
| Aspect | Gene Therapy | Traditional Treatments |
|---|---|---|
| Pain Management | Elimination of severe pain crises | Management of painful episodes through medication |
| Red Blood Cell Morphology | Improvement in the shape and function of red blood cells | No impact on red blood cell abnormalities |
| Curative Potential | Potential for long-term, possibly curative outcomes | Palliative care approach, managing the symptoms |
Preparing for a Stem Cell Transplant
Preparing for a stem cell transplant involves several important steps and procedures. These measures are taken to ensure the success of the transplant and minimize potential risks. Let’s take a closer look at how we prepare for a stem cell transplant.
HLA-Typing and Donor Selection
One of the crucial aspects of preparing for a stem cell transplant is HLA-typing. HLA refers to human leukocyte antigens, which are proteins that play a key role in the immune system. By analyzing the compatibility between the patient’s HLA markers and potential donors, we can determine the suitability of a donor for the transplant. Finding a suitable donor is critical for a successful transplant and a positive outcome.
Stem Cell Collection
The next step in the preparation process is stem cell collection. Stem cells are typically collected from the patient’s blood through a process called apheresis. During apheresis, blood is drawn from the patient’s body, the stem cells are separated from the other blood components, and the remaining blood is returned to the patient. This procedure may need to be repeated several times to collect enough stem cells for the transplant.
Conditioning
After the stem cells have been collected, the patient undergoes a conditioning regimen. Conditioning involves the use of high-dose chemotherapy or radiation therapy. The purpose of conditioning is to eliminate the patient’s existing stem cells and create space in the bone marrow for the transplanted stem cells to grow and function properly. However, it’s important to note that conditioning carries certain risks and potential side effects.
Research is ongoing to develop safer alternatives to traditional chemotherapy-based conditioning regimens. These alternatives aim to reduce the potential toxicity and complications associated with conditioning while maintaining the effectiveness of the transplant.
Additional Preparations
In addition to HLA-typing, stem cell collection, and conditioning, there are several other aspects involved in preparing for a stem cell transplant. These may include:
- Dental clearance to minimize the risk of infection during the transplant process.
- Pulmonary function tests to assess the patient’s lung health and ensure they can tolerate the transplant procedure.
- Various screenings and tests to evaluate the patient’s overall health and determine their eligibility for the transplant.
These additional preparations help ensure that the patient is in the best possible condition to undergo the transplant procedure and increase the chances of a successful outcome.
Managing Sickle Cell Disease and Complications
Individuals with sickle cell disease require lifelong management of their condition and prevention of complications. We understand the importance of pain management, infections prevention, and treating sickle cell-related anemia to enhance the quality of life for patients.
Pain Management
Pain management is crucial in providing relief from sickle cell crises, which are known to cause severe pain. There are various approaches to managing pain, including:
- Medications: Hydroxycarbamide and crizanlizumab are commonly prescribed to help manage pain in sickle cell disease patients.
- Prevention measures: Staying hydrated, wearing warm clothing, and avoiding sudden temperature changes can help prevent painful episodes.
Infections Prevention
Sickle cell disease impairs the immune system, making individuals susceptible to infections. To prevent infections, patients often require daily doses of antibiotics. Regular check-ups and vaccinations are also crucial to protect against common pathogens.
Treating Sickle Cell-Related Anemia
Anemia is a common complication of sickle cell disease. Treatment options for sickle cell-related anemia include:
- Folic acid supplements: These supplements help stimulate red blood cell production and combat anemia.
- Blood transfusions: In severe cases of anemia, blood transfusions may be necessary to maintain adequate oxygen supply to organs and tissues.
- Hydroxycarbamide: This medication can help increase the production of fetal hemoglobin, which improves red blood cell function and reduces anemia.
By focusing on pain management, infections prevention, and treating sickle cell-related anemia, we aim to alleviate the burden of sickle cell disease and improve the overall well-being of patients.
| Pain Management Options | Effectiveness | Side Effects |
|---|---|---|
| Hydroxycarbamide | Effective in reducing pain frequency and severity | Mild side effects such as nausea and skin changes |
| Crizanlizumab | Can significantly reduce pain episodes | Possible infusion reactions |
Source: Third source
Risks and Considerations of Stem Cell Transplants
Stem cell or bone marrow transplants offer the only cure for sickle cell disease, but they come with significant risks. It is important to be aware of these risks and consider them before undergoing a transplant.
Graft-versus-Host Disease (GVHD)
Graft-versus-host disease (GVHD) is a potentially life-threatening complication that can occur after a stem cell transplant. In GVHD, the transplanted cells recognize the recipient’s cells as foreign and attack them. This can lead to inflammation and damage to multiple organs, including the skin, liver, and gastrointestinal tract. GVHD can range from mild to severe, and it requires prompt medical intervention and treatment.
Conditioning Complications
Conditioning, which involves high-dose chemotherapy, is a crucial step in preparing the body for a stem cell transplant. While effective in eliminating existing stem cells and making room for the transplanted cells, conditioning can be toxic and cause various complications. These complications may include infection, organ damage, and even a small risk of developing cancer. Researchers are actively working on developing less toxic conditioning strategies to minimize these risks and improve the overall safety of the transplant process.
Stem cell transplants are generally considered for children with severe sickle cell disease who have not responded to other treatments. Suitable donors, especially fully matched siblings, increase the chances of a successful transplant. However, it is essential to thoroughly discuss the potential risks and benefits with healthcare professionals before making a decision.
Overall, while stem cell transplants offer hope for a cure, it is critical to understand and weigh the associated risks to make the best-informed decision for individual circumstances.
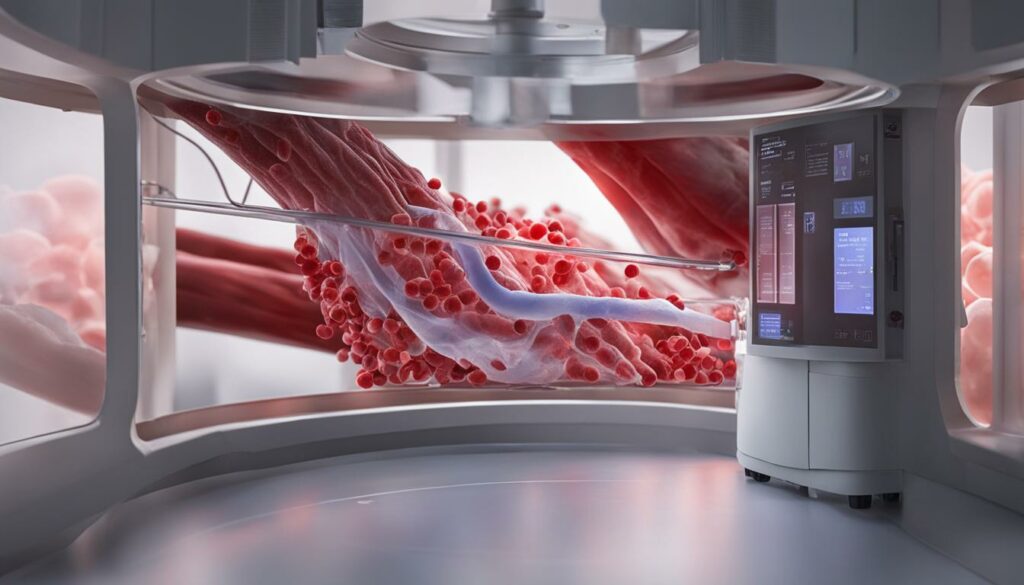
In this image, we see a visual representation of the risks involved in a stem cell transplant. The alt text for this image is “risks of stem cell transplant,” emphasizing the keyword related to this section.
Future Directions and Promising Advances
The field of gene therapy for sickle cell disease is witnessing exciting advancements and possibilities for the future. Researchers and scientists are making significant progress in developing new genetic approaches to cure the disease, aiming to improve the lives of individuals affected by sickle cell disease.
The Cure Sickle Cell Initiative, launched by the National Heart, Lung, and Blood Institute, is dedicated to accelerating the development of gene therapies for sickle cell disease. This initiative aims to provide hope for a future without the limitations imposed by this condition. Ongoing research in gene therapy focuses on finding safer alternatives to conditioning for stem cell transplants and making gene therapies more financially accessible.
Promising results have been observed in preclinical and clinical trials, demonstrating the potential of gene therapy in treating sickle cell disease. However, formal approval by regulatory bodies is still awaited, reflecting the rigorous evaluation processes to ensure safety and efficacy.
In addition to gene therapy, advancements in other areas such as stem cell transplantation are also contributing to the progress in sickle cell disease treatment. These advancements hold great promise for individuals living with sickle cell disease, offering potential cures and improved quality of life.
Financial Accessibility of Gene Therapies for Sickle Cell Disease
As gene therapies continue to evolve, one of the challenges is making them financially accessible to those who need them. The high costs associated with development, manufacturing, and delivery pose significant barriers for individuals with sickle cell disease.
Efforts are being made to address this issue and ensure equitable access to gene therapies. Collaborations between researchers, healthcare providers, and policymakers are crucial in advocating for affordable access to these life-changing treatments. Accessible pricing models, insurance coverage, and government initiatives are being explored to make gene therapies more affordable and available to a wider population.
By promoting financial accessibility, we can broaden opportunities for individuals with sickle cell disease to benefit from advancements in gene therapy and other innovative treatment modalities. Ensuring that cost is not a prohibitive factor will contribute to a more inclusive and equitable healthcare landscape.
Conclusion
Stem cell strategies, such as hematopoietic stem cell transplantation and gene therapy, offer promising possibilities for managing and potentially curing sickle cell disease. Despite the challenges involved, significant progress has been made in improving the quality of life for individuals with this condition. Ongoing research and advancements in stem cell therapies provide hope for a future free from the limitations imposed by sickle cell disease.
The availability of hematopoietic stem cell transplantation has proven to be a curative option for severe cases of sickle cell disease. However, it is essential to carefully weigh the potential benefits and risks associated with this procedure. Furthermore, gene therapy shows encouraging results in eliminating severe pain crises and improving the shape of red blood cells, offering new hope for individuals living with sickle cell disease.
Continued research efforts, such as the Cure Sickle Cell Initiative, are focused on developing new genetic approaches to cure the disease and finding safer alternatives to conditioning for stem cell transplants. The goal is to make these cutting-edge treatments more accessible and affordable, ensuring that individuals with sickle cell disease can benefit from the latest advancements in stem cell strategies.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic blood disorder caused by mutations in the beta-globin gene. It leads to the production of abnormal hemoglobin, causing red blood cells to deform and adopt a sickle-like shape when exposed to low-oxygen environments.
Is there a cure for sickle cell disease?
Currently, the only available curative therapy for sickle cell disease is hematopoietic stem cell transplantation (HSCT). HSCT can be autologous, involving genetic modification of the patient’s own stem cells, or allogeneic, using stem cells from a suitable donor.
What are the indications for HSCT in sickle cell disease?
HSCT is indicated in individuals with severe sickle cell disease and complications such as stroke, acute chest syndrome, recurrent pain crisis, nephropathy, and retinopathy. However, the decision to proceed with HSCT is complex and must consider potential benefits and risks.
What is gene therapy for sickle cell disease?
Gene therapy, such as LentiGlobin, is a promising treatment option for sickle cell disease. It involves the collection of the patient’s own blood-forming stem cells, followed by the delivery of a modified copy of the beta-globin gene into these cells. The modified stem cells are then reinfused into the patient’s bone marrow, where they start producing healthy red blood cells.
What preparations are required for a stem cell transplant?
Preparation for a stem cell transplant involves multiple tests and procedures. HLA-typing is performed to identify a suitable donor, and stem cells are collected from the patient’s blood. Conditioning, which involves high-dose chemotherapy, is necessary to eliminate old stem cells and make room for the modified stem cells.
How do you manage sickle cell disease and its complications?
The management of sickle cell disease includes measures to prevent painful episodes (sickle cell crises), such as staying hydrated, wearing warm clothing, and avoiding sudden temperature changes. Medications may be prescribed to manage pain, and individuals with sickle cell disease are often vulnerable to infections and require daily doses of antibiotics.
What are the risks and considerations of stem cell transplants?
Stem cell or bone marrow transplants are the only cure for sickle cell disease but carry significant risks. Graft-versus-host disease (GVHD) is a life-threatening complication, and conditioning with high-dose chemotherapy can be toxic. Suitable donors, such as fully matched siblings, increase the chances of a successful transplant.
What are the future directions and advances in sickle cell disease treatment?
The field of gene therapy for sickle cell disease is advancing rapidly. Ongoing research focuses on finding safer alternatives to conditioning for stem cell transplants and making gene therapies financially attainable. Promising results have been seen in preclinical and clinical trials, but formal approval by regulatory bodies is still awaited.
What are the possibilities for managing sickle cell disease?
Stem cell approaches, including hematopoietic stem cell transplantation and gene therapy, hold promise for the future of sickle cell disease treatment and potential cure. Despite the challenges, significant progress has been made in managing the disease and improving quality of life for individuals with sickle cell disease.
