Imagine your joints as the hinges on a well-used door; over time, they can start to creak and wear down, making every movement a bit more strenuous. This is the reality for those living with osteoarthritis (OA), a degenerative joint disease that leads to the breakdown of joint cartilage and underlying bone. It’s a condition that can turn the simple act of climbing stairs into a challenge. While there’s no shortage of treatments, from painkillers to joint replacement surgery, they often come with limitations and side effects. This is where mesenchymal stem cells (MSCs) step into the spotlight, offering a potential new therapeutic avenue for those seeking relief from the relentless march of OA.
In this article, we’ll explore the role of MSCs in treating osteoarthritis, particularly focusing on severe osteoarthritis of the knee, a common battleground for this condition. We’ll delve into the science behind MSC therapy, the procedure itself, and the benefits and risks associated with it. Whether you’re a patient considering this therapy for osteoarthritis or simply curious about the latest advancements in regenerative medicine, join us as we unpack the exciting potential of MSCs.
Understanding Osteoarthritis
The Mechanics of a Worn-Out Joint
Osteoarthritis is like the erosion of a once-smooth pathway, where the cartilage that cushions the joints wears down over time. This can lead to pain, stiffness, and other symptoms that can severely impact daily life.
Symptoms and Diagnosis
The journey of living with OA often begins with stiffness in the morning, a twinge of pain when standing up, or a persistent ache that won’t go away. Diagnosis typically involves a combination of patient history, physical examination, and imaging tests like X-rays or MRIs.
Current Treatments and Their Limits
The current arsenal against OA includes pain relievers, anti-inflammatory drugs, physical therapy, and, in severe cases, surgery. However, these treatments often offer temporary relief and can come with side effects.
The Science of Mesenchymal Stem Cells
A Closer Look at MSCs
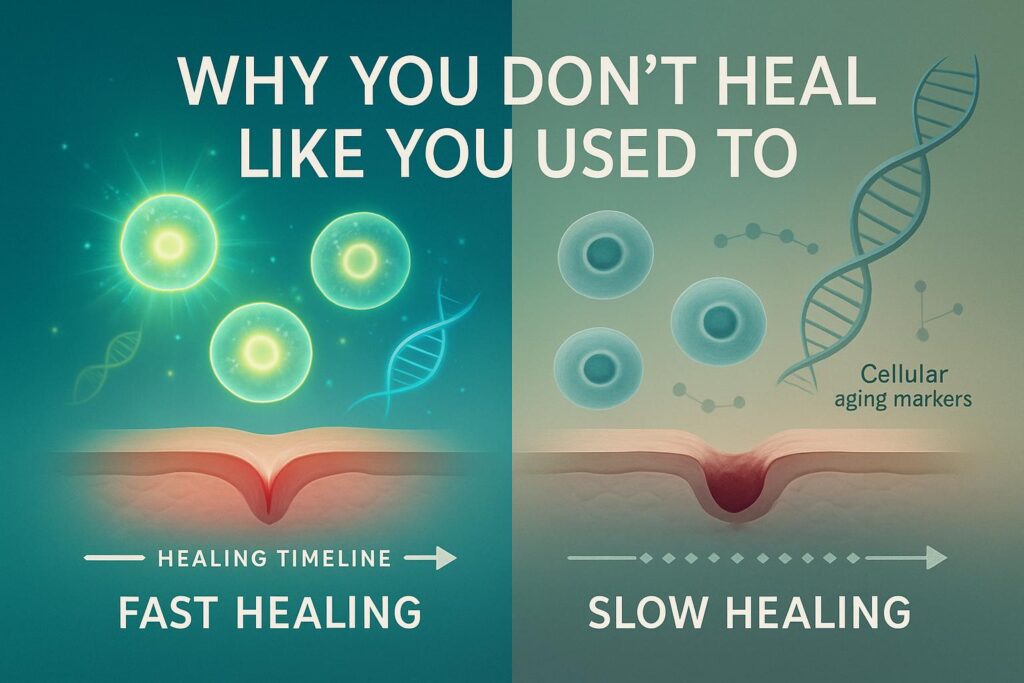
Human mesenchymal stem cells are like the body’s own repair technicians. They have the remarkable ability to differentiate into a variety of cell types and have therapeutic applications in numerous diseases, including OA.
Tissue Regeneration: The MSC Superpower
One of the most compelling properties of MSCs is their ability to promote tissue repair and regeneration. They’re like the construction workers of the cellular world, rebuilding damaged structures within the body.
Harvesting MSCs: The Source Matters
MSCs can be sourced from various tissues, such as bone marrow, adipose tissue, and even umbilical cord blood. Each source has its own advantages and potential applications in stem cell therapy.
Comparing Sources of Mesenchymal Stem Cells
When considering mesenchymal stem cell therapy for conditions like osteoarthritis, it’s important to understand that not all MSCs are created equal. The source of these cells can significantly influence their characteristics and therapeutic potential. Let’s explore the differences between bone marrow mesenchymal stem cells (BM-MSCs), adipose-derived mesenchymal stem cells (AD-MSCs), and umbilical cord-derived mesenchymal stromal cells (UC-MSCs).
Bone Marrow Mesenchymal Stem Cells (BM-MSCs)
BM-MSCs are the traditional stalwarts in the field of MSC therapy. Harvested from the bone marrow, a process that can be invasive and painful, these cells are well-studied and have a proven track record in regenerative medicine.
- Differentiation Potential: BM-MSCs have a high differentiation potential, meaning they can transform into a variety of cell types, including bone, cartilage, and fat cells.
- Availability: They are less abundant than other types of MSCs, which can make them more challenging to collect in large numbers.
- Therapeutic Use: BM-MSCs have been used in numerous clinical trials and are known for their ability to support the regeneration of bone and cartilage, which is particularly relevant in the treatment of osteoarthritis.
Adipose-Derived Mesenchymal Stem Cells (AD-MSCs)
AD-MSCs are obtained from adipose tissue, commonly known as body fat. This source is less invasive to harvest from compared to bone marrow and yields a higher number of MSCs.
- Differentiation Potential: While they share similar properties to BM-MSCs, AD-MSCs may have a greater propensity for fat cell differentiation.
- Ease of Collection: The extraction process from adipose tissue is generally less painful and provides a larger quantity of MSCs, making it a more patient-friendly option.
- Therapeutic Applications: These cells are being studied for their effectiveness in treating a wide range of conditions, including osteoarthritis of the knee.
Umbilical Cord-Derived Mesenchymal Stromal Cells (UC-MSCs)
UC-MSCs are a newer area of interest, sourced from the umbilical cord tissue, which is typically discarded after birth. These cells are considered to be more “primitive” and may have unique advantages.
- Immunomodulatory Properties: UC-MSCs are noted for their strong immunomodulatory abilities, which can be beneficial in reducing inflammation.
- Ethical Considerations: The use of UC-MSCs avoids some of the ethical concerns associated with embryonic stem cells, as they are harvested from a waste product after birth.
- Clinical Potential: Research into UC-MSCs is ongoing, but they show promise for use in a variety of therapeutic applications due to their robust growth and differentiation capabilities.
In summary, while all three types of MSCs hold promise for the treatment of osteoarthritis and other conditions, they each come with distinct features that may make them more suitable for specific applications. Ongoing clinical trials and research will continue to clarify their roles and optimize their use in regenerative medicine.
MSCs in the Treatment of Osteoarthritis
How MSCs Can Help
Mesenchymal stem cells offer a multifaceted approach to treating OA. They can potentially regenerate cartilage, reduce inflammation, and release molecules that promote healing within the joint.
From Bench to Bedside: Clinical Trials
A growing body of clinical trials is examining the effectiveness of MSCs in treating osteoarthritis. These studies are crucial in translating MSC therapy from a promising concept into a real-world treatment.
The Evidence: Clinical Outcomes
The results from clinical trials have been promising, with many showing improvements in pain and joint function. However, it’s important to note that MSC therapy is still an emerging field, and ongoing research is needed to fully understand its potential.
The Procedure of MSC Therapy for OA
Preparing for MSC Therapy
Before undergoing MSC therapy, patients undergo a thorough evaluation to determine if they are suitable candidates. This is akin to preparing the ground before planting a new seedling.
The Step-by-Step Guide to MSC Therapy
The actual therapy involves extracting MSCs, often from the patient’s own body, and then injecting them into the affected joint. Think of it as planting seeds in a garden where the soil has become barren, in hopes of reviving the landscape.
Aftercare: Nurturing the New Growth
Post-treatment care is crucial for ensuring the best possible outcome from MSC therapy. Patients may need to follow specific guidelines to allow the stem cells to integrate and exert their effects.
Benefits and Risks of MSC Therapy in OA
Weighing the Pros and Cons
MSC therapy offers a beacon of hope for many, with the potential to not only alleviate symptoms but also to address the underlying damage in OA. However, as with any medical treatment, it comes with its own set of risks and considerations.
Understanding the Risks
While MSC therapy is generally considered safe, there is a risk of infection, and the long-term outcomes are still being studied. It’s like embarking on a new trail; the path is promising, but we must proceed with caution.
The Success Stories
Many patients have reported significant improvements in their quality of life following MSC therapy. These anecdotes serve as encouraging signs of the therapy’s potential, lighting the way for future advancements.
Patient Considerations for MSC Therapy
Is MSC Therapy Right for You?
Not everyone with OA will be a candidate for MSC therapy. Factors such as the severity of the disease, overall health, and previous treatments will all play a role in determining eligibility.
The Cost of Innovation
While MSC therapy represents a cutting-edge treatment option, it can also come with a significant price tag. Patients must consider the financial implications alongside the potential benefits.
The Ethical Landscape
The use of stem cells in medicine is a topic of ethical debate. It’s important for patients to understand the source of the stem cells being used and the ethical standards upheld by the treating facility.
The Future of MSC Therapy in OA
The Road Ahead
The field of MSC therapy is rapidly evolving, with new research shedding light on how these cells work and how they can be optimized for treating conditions like OA.
Personalized Medicine: Tailoring Treatment
In the future, MSC therapy may become more personalized, with treatments tailored to the individual’s specific condition and needs. It’s like having a suit custom-made rather than off-the-rack; the fit is just better.
Combination Therapies: The Power of Teamwork
Researchers are also exploring the use of MSCs in combination with other therapies to enhance their effectiveness. This approach is like using both a map and a compass on a hike; each tool adds value to the journey.
FAQ
Q: What are mesenchymal stem cells (MSCs)?
A: Mesenchymal stem cells (MSCs) are a type of adult stem cells that can be found in various tissues of the body, including bone marrow, adipose tissue, and synovial fluid. They have the ability to differentiate into different cell types and can be used in regenerative medicine.
Q: What are the therapeutic properties of mesenchymal stem cells?
A: Mesenchymal stem cells have several therapeutic properties that make them promising for the treatment of various medical conditions. These properties include their immunomodulatory effects, anti-inflammatory properties, and their ability to promote tissue repair and regeneration.
Q: How can mesenchymal stem cells be used in osteoarthritis therapy?
A: Mesenchymal stem cell therapy has shown promising results in the treatment of knee osteoarthritis. The stem cells can be derived from various sources, such as bone marrow or adipose tissue, and are then injected into the affected joint. These stem cells can help reduce inflammation, promote tissue regeneration, and potentially slow down the progression of the disease.
Q: What are the different sources of mesenchymal stem cells?
A: Mesenchymal stem cells can be derived from various sources, including bone marrow, adipose tissue, and synovial fluid. Each source has its advantages and disadvantages, and the choice of source depends on factors such as availability, processing time, and therapeutic potential.
Q: How do bone marrow-derived mesenchymal stem cells differ from adipose-derived mesenchymal stem cells?
A: Bone marrow-derived mesenchymal stem cells and adipose-derived mesenchymal stem cells are two different sources of mesenchymal stem cells. While both sources have similar differentiation potential and therapeutic properties, there may be slight differences in terms of cell yield, processing time, and ease of isolation.
Q: Are there any clinical trials on the use of mesenchymal stem cells for osteoarthritis?
A: Yes, there have been several clinical trials evaluating the use of mesenchymal stem cells for the treatment of knee osteoarthritis. These trials have shown promising results, with improvements in pain, function, and quality of life observed in many patients. However, more research is still needed to determine the long-term effectiveness and safety of this therapy.
Q: How do mesenchymal stem cells compare to hyaluronic acid for osteoarthritis treatment?
A: Mesenchymal stem cells and hyaluronic acid are two different treatment options for knee osteoarthritis. While hyaluronic acid provides temporary relief by lubricating the joint, mesenchymal stem cells have the potential to promote tissue repair and regeneration. Studies comparing the two treatments have shown mixed results, and the choice between them depends on factors such as the severity of the condition and individual patient preferences.
Q: What is the current status of mesenchymal stem cell therapy in osteoarthritis treatment?
A: Mesenchymal stem cell therapy shows great potential for the treatment of knee osteoarthritis. However, it is still considered an experimental treatment and is not yet widely available. This therapy is mainly being performed in the context of clinical trials and should be discussed with a qualified healthcare professional.
Q: Are there any risks or side effects associated with mesenchymal stem cell therapy?
A: The risks and side effects of mesenchymal stem cell therapy are generally low. The procedure itself is minimally invasive, and the cells used are often autologous (meaning they are derived from the patient’s own body), which reduces the risk of rejection or adverse reactions. However, as with any medical procedure, there is a small risk of infection, bleeding, or allergic reactions.
Q: Is mesenchymal stem cell therapy covered by insurance?
A: Currently, mesenchymal stem cell therapy for knee osteoarthritis is not covered by most insurance plans. Since it is still considered an experimental treatment, patients may need to bear the costs themselves. It is recommended to check with your insurance provider for specific coverage details.
Conclusion
The exploration of human mesenchymal stem cells in the realm of therapy for osteoarthritis is an exciting frontier in medicine. With each clinical trial and every patient’s story, we inch closer to understanding the full potential of MSCs. For those considering stem cell therapy, it’s a path worth exploring with the guidance of healthcare professionals.
As we continue to navigate this new terrain, the promise of MSCs shines like a beacon, offering hope for a future where the creaks and groans of worn-out joints are but a distant memory.