International Guest Speaker, Dr. William Murrell joins Dr. Rogers and Dr. Ambach in this webinar and shares his experience and knowledge as an orthopedic surgeon in the use of cell therapy and surgery for knee joint pain.
Video Transcript (partial):
Thanks good to see you folks joining us today for those of you that are regulars, we have a special treat for you today, uh I’m Dr Christopher Rogers. That’s not the special treat. Dr Ambach is joining me as well today where we talk about cell therapies versus surgical care for knee joint pain.
Um, we’re gonna talk, we’re gonna introduce a little bit later a friend of ours, Dr Bill Murrell, an orthopedic surgeon who is well known. He lectures all over the world and so we’re bringing him to San Diego today and he’s going to share with us some of the special things that he’s been working on.
Yeah thanks. Everyone for joining us um we’re excited to have Dr Murrell. He is an international guest speaker and I think you’ll learn a lot from him being an orthopedic surgeon and sharing his knowledge, experience, and insights on this non-invasive, non-surgical treatment options for knee joint pain.
So Dr Rogers and I will do a quick introduction slides to his lecture most of the time for this webinar was um, was reserved for his presentation and then we’re gonna follow that with a question and answer portion.
So, while listening to the lecture, if you do have any questions, just go ahead and type it into that chat button at the bottom of your screen and then after we’re done with the presentation, we’ll get to those questions and answer them one at a time. Dr Murrell will also answer questions on the topic after the talk.
Great. So, as I mentioned, I’m Christopher Rogers, I’m a physician here in San Diego, been in practice for 23 years, board certified in what’s called physical medicine rehabilitation, as is Dr Ambach. We’re both physiatrists, which is a non-surgical specialty that focuses on the musculoskeletal system. So we’re experts in non-surgical orthopedic care. We are both fellowship trained, I’m fellowship trained in sports and spine and, as is Dr Ambach, which means that we resisted the urge to get a job after residency and we decided to do one more year of training. We were both blessed to work with very talented physicians who trained us back, uh for me, it was back in 1997.
We’ve been lecturing on regenerative medicine now for at least the last eight years and that’s actually how I have met Dr Ambach. So we like to do research, we like to publish book chapters, we like to give lectures, we like to teach workshops, so we’re very involved in the regenerative medicine community, which is where we get to meet a lot of great people and train the next generation of Physicians, who will hopefully integrate these new therapies into their toolbox as they treat their patients.
Last year we conducted a FDA approved clinical trial for knee osteoarthritis using stem cells from a patient’s own body, and that report was just recently submitted to FDA and we’re going to be moving forward to a phase II randomized clinical trial probably early this summer.
Dr Ambach was also a participant in a multi-center randomized clinical trial looking at treating patients with chronic low back pain and disc degeneration using cell-based therapies and we’ll be talking a little bit about some of these cell-based therapies.
Our special guest today, which we’ll introduce in a little bit, Dr William Murrell, is a board-certified orthopedic surgeon. You know we get a lot of questions by the way, as non-surgeons doing innovative therapy.
What do the orthopedic surgeons think about this new medicine?
These new cell therapies and the potential for them to replace some of the existing orthopedic surgeries that are performed, such as a meniscectomy or a joint replacement, and I always answer the same way. I say the more progressive ones who understand cell therapy, realize that this is the future of orthopedic care and they embrace the technology. Not only do they embrace the technology but they’re pushing it forward by conducting research. So this is how we met Dr Murrell, he’s a shining star in the field, he’s also fellowship trained in sports medicine, where he specializes. He’s a consultant and director of the orthopedic center of excellence in UAE, and he’s the president and founder of the American Academy and American Board of Regenerative Medicine, which is a new organization that brings together different positions of different specialties who have an interest in regenerative medicine. And then he founded the Dubai Sports Medicine Center, which is a real premier, world-class facility that brings a lot of the technologies that aren’t even available in the United States yet, and brings a lot of expertise to that area.
So we’re going to first start with a basic introduction to cell-based therapies for joint pain and then we’ll talk about some of the surgical options as well. We’ll hear from Dr Murrell and then at the end we’ll take your questions.
So our company is called San Diego Orthobiologics Medical Group. Orthobiologics is a term that we want everybody to learn. It simply refers to orthopedic treatments that involve the use of cells or substances, molecules that are derived from cells, and it’s based on the premise that in regenerative medicine we understand that the body has a natural ability to heal itself, and so we’re just learning how that happens and we’re augmenting those processes to help injuries that are having trouble healing.
Some of the common orthobiologics you may have heard about – are platelets, which are cells in your blood stem cells. I’m sure you’ve heard about, but you may not have heard about some of these growth factors cytokines or other molecules that the cells manufacture in their attempt to help heal injured tissues uh. This is um a little uh shout out to our youtube channel uh. If you just can’t get enough of us, go to youtube and type in san diego orthobiologics, and we have probably now 20 or 30 lectures on there for you to view at your leisure. These particular lectures talk about some of the more common ortho biological therapies that we offer. These are cell therapies, derived from your own fat tissue, adipose tissue uh from your own bone marrow tissue or from your own platelets from your own blood. So you can watch those at your leisure. Probably the most common thing that we do in our office would be something called PRP or platelet-rich plasma platelets. We don’t do a cookie cutter approach. Everybody gets their own customized version. You can see also I have a cell counter, so we can measure the dose of cells that we’re giving you. These cells release growth factors that stimulate your tissues to heal. They form new blood vessels. They call stem cells into the injured tissues to help with the healing. They also decrease inflammation in a lot of ways. They might function like cortisone where you decrease inflammation in an irritated joint. The difference is it’s safer and it lasts longer.
Next slide. As I mentioned, we customize our PRP. There’s at least 37 different flavors of PRP. The most common flavors are cranberry, orange, and pineapple. Uh, I’m kidding – they don’t taste like flavors, but you can tell that some of the PRP may have more red blood cells in it, giving it that red color and some have fewer red blood cells, making it more of a pineapple juice color. So, for example, in the knee joint, we don’t we don’t want to inject red blood cells into the joint. The iron, the hemoglobin in the red cells is not good for your cartilage, and so, if you’re going to have PRP injected into your knee joint, make sure it’s not the red bloody kind. We would use that more for a wound or for a um, really stubborn, tendon tear.
What Are Stem Cells?
Now Dr Ambach, can you tell us about stem cells?
Yeah, so there are more than 37 trillion cells in our body, and these cells are constantly dying and being replaced and stem cells are responsible for replacing lost cells due to either injury, wear and tear diseases or other reasons wherein we lose some of these cells. Um stem cells are unique in the sense that they don’t just have the ability to renew themselves and help us grow. You know, as our physical bodies grow from a kid to a an adult person, but they also turn into other cell types, depending on what our body needs and they’re the only one of these cells that can do this in orthopedics.
We are particularly interested in adult stem cell, that’s called mesenchymal stem cells, and this is a specific type of adult stem cell that can differentiate into other cell types that are useful in orthopedics, like muscle tissue, cartilage tissue, um, bone tissue, fats, blood vessels and nerves.
Dr Arnold Caplan, which is the gentleman here in the middle in the picture on the upper left here, is the father of MSC and he named mesenchymal stem cells about 25 years ago. So these MSCs just lie or live around our small blood vessels in our body, just waiting to be activated whenever they’re needed and once they’re activated, they release hundreds and hundreds of molecules. They act like a drug stores. Basically, they release these natural drugs and molecules from our body that serves many functions, some of which involve tissue healing controlling inflammation fighting infection and helping with pain. The stem cells that we use in clinic are derived from either the bone marrow or adipose tissue, which is not processed by enzymes. These tissues are what we used in the clinic. They are compliant with current FDA regulations regarding the use of cells in the office. Cell-Based therapies, um as a whole have um a lot of studies to support its use. I know it’s a completely a separate lecture just to go over data and evidence on its use, but it’s got hundreds of our research proving that it’s safe to use um that it helps decrease, inflammation and pain, uh increase in function. They will also have clinical research to show how it works, and we have discussed some of the mechanisms by how it works, and this is to stimulate tissue repair, increase blood flow help with the pain and fight infection.
So we’re going to start with Dr Murrell’s lecture and we’re going to finish that lecture and then finish it with the question and answer portion today.
We’re going to talk about cellular therapy versus surgery for knee joint pain. Here are my affiliations and disclosures. I currently work at Healthpoint Hospital Abu Dhabi Knee and Sports Medicine Center, a pretty big facility. We have 15 orthopedic surgeons, divided between upper and lower extremity about 50 physical therapists. We have over 1200 outpatient visits today over 200 surgeries done per month. Today’s main points in this talk will focus on uh four areas. One really, the main issue to addressing most knee joint pain is lifestyle related issues. This will be the talked about the first part of my talk uh. The other point is that most of the problems that we see for the knee joint can be managed uh with non-interventional non-operative treatment, most of the minimally invasive interventional therapeutic options like orthobiologics and other cellular-based therapies can work for most individuals most of the time.
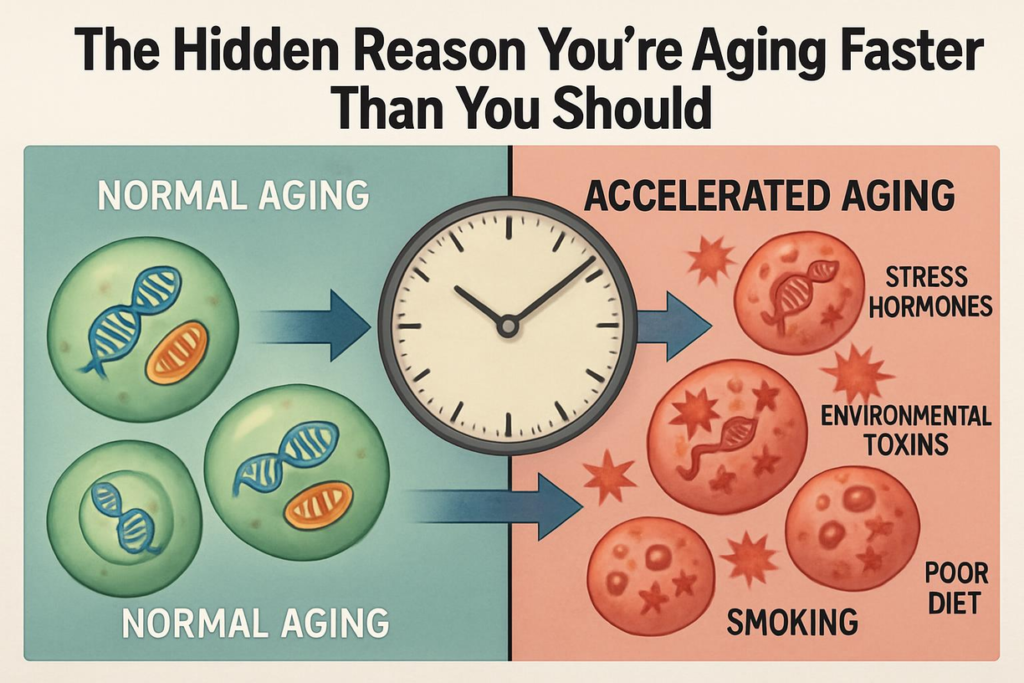
Other times, invasive interventional procedures, like surgery, can also use orthobiologics in many instances, but for the most part at least in my hands, most procedures are done non-surgically and I’m an orthopedic surgeon. I’ve been in practice for about 20 years and I’m going to make a prediction prior to the start of this talk; and that is by 2040 I think that we will become much more effective at treating the primary problem, which is lifestyle for many locations in the world, maybe not San Diego, but certainly around the world. We’re dealing with issues related to lifestyle most of the time and what I’ve seen in my own practice since 2008, where I would do four to 600 cases a year I found that most of my cases in 20 up to 2018 have become interventional about 72 of the cases that i do are now interventional and and as an orthopedic surgeon, we do involve ourselves in the uh managing lifestyle related issues because we’re doctors too, and it’s just not about doing surgery. Managing lifestyle is about choices and we can choose to eat well and rest and take adequate water and eat right foods, uh non-processed foods. This is really our choice: uh we can do the things that feel good, and these things have consequences, and these consequences is one of the consequences is obesity.
I know this may not be a big issue in San Diego, but in many places in the US, as well as the UK, here in the middle east, we have major problems with obesity. And what are the major issues with this? Well, when you’re obese, you have marked effects on your genetics and your genetic stability. And so when you, your genes, are unstable, all the proteins that govern all the biological processes in your body, the meta metabolism and such become unstable.
So the proteins that your body makes don’t work, and when they don’t work, things like generating energy, even though you have an excess of energy stored in the body, your mitochondria are poisoned and they can’t even make energy to do the normal processes of the body. And this is why a lot of people that are obese are quite tired and being obese has had a huge impact on the prevalence of osteoarthritis.
*** All content on NationalStemCellTherapy.com is for informational purposes only. All medical questions and concerns should always be consulted with your licensed healthcare provider.