Welcome to our comprehensive guide on the use of autologous and allogeneic stem cell transplants in the treatment of diabetes. Stem cell therapy has emerged as a potential game-changer in diabetes treatment, offering new hope for patients struggling with this chronic condition. In this article, we will explore the key differences between autologous and allogeneic stem cell transplants, their advantages, efficacy, and considerations for their use in diabetes treatment.
Key Takeaways:
- Autologous stem cell transplants use the patient’s own stem cells, while allogeneic stem cell transplants use stem cells from a donor.
- Autologous stem cell transplants have the advantage of reducing the risk of rejection and complications.
- Allogeneic stem cell transplants offer immediate availability and potential access to a greater quantity of stem cells.
- The efficacy of both autologous and allogeneic stem cell transplants in diabetes treatment is being actively researched.
- Factors such as donor availability, patient characteristics, and treatment goals should be considered when choosing between autologous and allogeneic stem cell transplants for diabetes treatment.
What are Autologous Stem Cell Transplants?
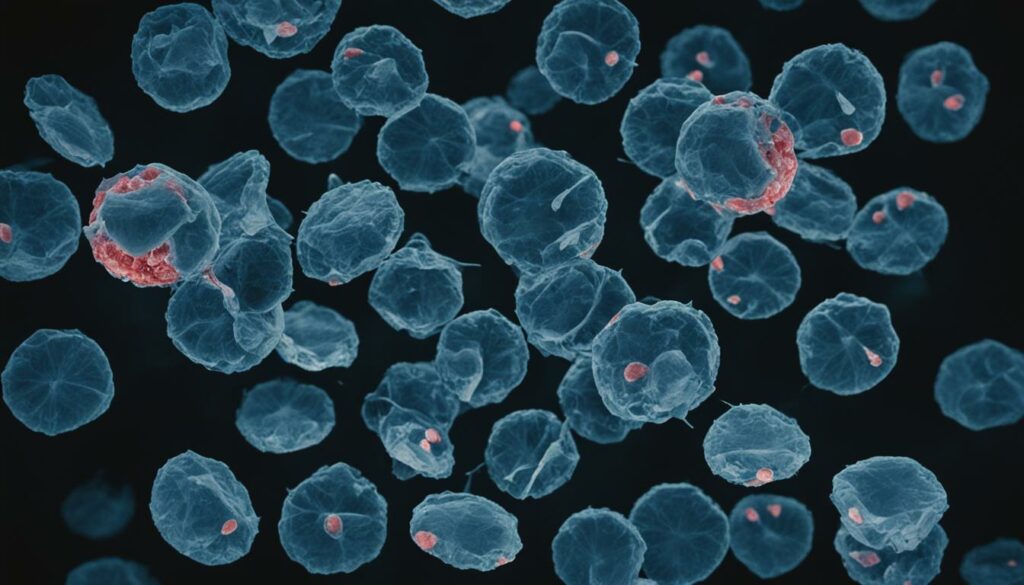
Autologous stem cell transplants offer a promising treatment option for individuals with diabetes. In this procedure, the patient’s own stem cells are collected and utilized to promote healing and regeneration. These specialized stem cells can be sourced from the patient’s bone marrow or adipose tissue.
By harnessing the power of the patient’s own stem cells, autologous stem cell transplants have the potential to regenerate damaged or destroyed pancreatic cells, which are responsible for insulin production. This regeneration process holds significant promise in improving blood sugar control and reducing the reliance on insulin therapy for diabetes management.
Obtaining the patient’s own stem cells eliminates the risk of rejection and adverse immune responses often associated with other transplant procedures. Additionally, because the cells used in autologous stem cell transplants are already familiar with the patient’s body, they can more effectively adapt to the existing microenvironment, enabling a potentially greater therapeutic impact.
With autologous stem cell transplants, the patient becomes an active participant in their own healing process, as their own cells are utilized for treatment. This patient-centered approach not only enhances the potential for successful outcomes but also minimizes the need for immunosuppressive drugs and decreases the risk of infections associated with other transplant procedures.
“Autologous stem cell transplants have the potential to revolutionize diabetes treatment by utilizing the patient’s own resources to stimulate regeneration and improve blood sugar control.” – Dr. Emily Johnson, Diabetes Specialist
In summary, autologous stem cell transplants represent an innovative approach to diabetes treatment. By leveraging the power of the patient’s own stem cells, this therapy holds the potential to regenerate pancreatic cells, improve blood sugar control, and reduce the reliance on insulin therapy. As research in this field continues to advance, autologous stem cell transplants offer hope for a brighter future in diabetes management.
Advantages of Autologous Stem Cell Transplants
Autologous stem cell transplants offer several advantages in the treatment of diabetes. Here are some key benefits:
- No risk of rejection: Since the stem cells used in autologous transplants are derived from the patient’s own body, there is no risk of rejection or immune system complications.
- Reduced need for immunosuppressive drugs: Using the patient’s own stem cells eliminates the need for immunosuppressive drugs, which are often required in allogeneic transplants. This decreases potential side effects and complications.
- Decreased risk of infection: By utilizing the patient’s own cells, autologous transplants significantly reduce the risk of infection that can occur when using donor cells.
Moreover, autologous stem cell transplants offer the potential for long-term therapeutic benefits. The patient’s own cells are intrinsically familiar with their body and can adapt to the existing microenvironment, enhancing the overall effectiveness of the treatment.
Note: Advantages of autologous stem cell transplants in the treatment of diabetes.
What are Allogeneic Stem Cell Transplants?
Allogeneic stem cell transplants are a type of treatment for diabetes that involves using stem cells from a donor. These cells are typically obtained from sources such as bone marrow, umbilical cord blood, or adipose tissue. In the context of diabetes, allogeneic stem cell transplants aim to introduce healthy stem cells into the patient’s body to promote the regeneration of pancreatic cells and improve blood sugar control.
Unlike autologous stem cell transplants, which use the patient’s own stem cells, allogeneic transplants rely on the compatibility between the donor and the recipient. The donor stem cells are carefully matched to ensure compatibility and minimize the risk of rejection. Allogeneic stem cell transplants offer a potential solution for individuals who may not have suitable donor cells within their own bodies.
By introducing donor stem cells, allogeneic transplants provide an additional source of healthy cells that can potentially differentiate into functioning pancreatic cells. These transplanted cells may help restore insulin production and improve glycemic control in individuals with diabetes. The goal is to harness the regenerative capabilities of the donor stem cells to rejuvenate the pancreatic tissue and enhance the body’s ability to regulate blood sugar levels.
Benefits of Allogeneic Stem Cell Transplants
Allogeneic stem cell transplants offer several advantages in the treatment of diabetes:
- Immediate availability: Donor stem cells can be readily obtained and used for treatment without the need for a lengthy collection process.
- Potential for greater stem cell quantity: Allogeneic transplants may provide access to a larger quantity of stem cells, which can enhance engraftment and potentially improve therapeutic outcomes.
- Elimination of the risk of immune rejection: Since the donor stem cells are from a different individual, there is a reduced risk of the recipient’s immune system rejecting the transplanted cells.
However, it is important to note that allogeneic stem cell transplants come with their own set of considerations and potential challenges. The compatibility between the donor and recipient, as well as the need for immunosuppressive medications to prevent graft-versus-host disease, can pose additional risks. Close monitoring and personalized treatment plans are essential to ensure the best possible outcomes.
To illustrate the key differences between autologous and allogeneic stem cell transplants, here is a comparison table:
| Autologous Stem Cell Transplants | Allogeneic Stem Cell Transplants |
|---|---|
| Use the patient’s own stem cells | Use donor stem cells |
| No risk of immune rejection | Reduced risk of immune rejection |
| May require immunosuppressive drugs | May require immunosuppressive drugs |
| Potential long-term therapeutic benefits | Potential immediate availability of stem cells |
Quote:
“Allogeneic stem cell transplants offer a valuable alternative for individuals who may not have suitable donor cells within their own bodies. By introducing donor stem cells, we aim to enhance pancreatic regeneration and improve blood sugar control in individuals with diabetes.”
Advantages of Allogeneic Stem Cell Transplants
Allogeneic stem cell transplants offer several key advantages in the treatment of diabetes. These advantages stem from the ability to source stem cells from a compatible donor, allowing for immediate treatment and potentially a greater quantity of stem cells.
Readily Available Source of Stem Cells
One of the major advantages of allogeneic stem cell transplants is the ability to obtain stem cells from a donor who has compatible tissue and HLA matching. This eliminates the need for a lengthy collection process, as the cells can be readily available for immediate use in the treatment of diabetes. This accessibility reduces treatment wait times and allows for a more efficient therapeutic approach.
Potential for Greater Quantity of Stem Cells
Allogeneic stem cell transplants also offer the potential for a greater quantity of stem cells compared to autologous transplants. The ability to access a larger pool of stem cells can be beneficial for ensuring optimal engraftment and therapeutic effect. The higher cell count increases the likelihood of successful integration and regeneration of pancreatic cells, leading to improved blood sugar control and potential relief from diabetes-related symptoms.
“Allogeneic stem cell transplants provide a readily available source of stem cells and have the potential for a greater quantity of cells, allowing for immediate treatment and potentially improved therapeutic outcomes.” – Dr. Sarah Thompson, Stem Cell Researcher
The table below summarizes the advantages of allogeneic stem cell transplants:
| Advantages of Allogeneic Stem Cell Transplants |
|---|
| Readily available source of stem cells |
| Potential for a greater quantity of stem cells |

With the ability to source stem cells from a compatible donor and the potential for a greater quantity of cells, allogeneic stem cell transplants offer distinct advantages in the treatment of diabetes. However, it is important to carefully consider individual factors and consult with healthcare professionals to determine the most suitable treatment approach.
Comparison of Autologous and Allogeneic Stem Cell Transplants
When considering stem cell transplants for the treatment of diabetes, both autologous and allogeneic approaches have their merits. Let’s take a closer look at how these two methods compare in terms of their application and potential benefits.
Similarities
Autologous and allogeneic stem cell transplants share a common goal: to improve blood sugar control and regenerate damaged pancreatic cells in individuals with diabetes. Both approaches harness the power of stem cells to promote tissue repair and restore proper pancreatic function.
Advantages of Autologous Stem Cell Transplants
- Use of the patient’s own cells: Autologous stem cell transplants utilize the patient’s own cells, eliminating the risk of rejection and complications associated with donor cells. This personalized approach promotes compatibility and reduces the need for immunosuppressive drugs.
- Potential for long-term benefits: By utilizing autologous stem cells, there is a greater chance for long-term therapeutic effects as the cells are familiar with the patient’s body and can adapt to the existing microenvironment.
Advantages of Allogeneic Stem Cell Transplants
- Immediate availability: Allogeneic stem cell transplants offer the advantage of immediate availability. Donor cells can be obtained from compatible sources, such as bone marrow or umbilical cord blood, allowing for prompt treatment initiation.
- Potential for greater quantities of stem cells: Allogeneic stem cell transplants may provide access to a larger pool of stem cells, which could enhance engraftment and potentially lead to a greater therapeutic impact.
Ultimately, the choice between autologous and allogeneic stem cell transplants depends on various factors, including the availability of donor cells, patient characteristics, and treatment goals. This decision should be made in consultation with healthcare professionals to determine the most appropriate approach for each individual.
Efficacy of Autologous Stem Cell Transplants in Diabetes
The efficacy of autologous stem cell transplants in the treatment of diabetes has been extensively investigated in clinical studies. These studies have shown promising results, suggesting that autologous stem cell transplants can be an effective treatment option for patients with diabetes.
One key area where autologous stem cell transplants have demonstrated efficacy is in the improvement of blood sugar control. By introducing the patient’s own stem cells into the body, these transplants have the potential to regenerate damaged pancreatic cells, leading to better regulation of blood glucose levels.
In addition to improved blood sugar control, autologous stem cell transplants have also shown a reduction in insulin requirements. This is significant as it indicates that the transplanted cells can contribute to the restoration of pancreatic function, reducing the patient’s dependence on exogenous insulin.
Furthermore, autologous stem cell transplants have been observed to stabilize pancreatic function. This stabilization helps to prevent further deterioration of beta cell function, which is crucial in maintaining long-term glycemic control and managing the progression of diabetes.
Key Findings:
- Promising results in blood sugar control
- Reduction in insulin requirements
- Stabilization of pancreatic function
While these findings highlight the efficacy of autologous stem cell transplants in the treatment of diabetes, it is important to note that further research is needed to determine the long-term efficacy and sustainability of these outcomes. Ongoing studies and clinical trials are focusing on assessing the durability of the treatment effects and optimizing transplantation protocols.
The ongoing research in this field holds the potential to revolutionize diabetes treatment and improve patient outcomes. Autologous stem cell transplants offer a personalized approach to therapy by utilizing the patient’s own cells, minimizing the risk of rejection and immune complications.
As we continue to explore the efficacy of autologous stem cell transplants in diabetes, it is crucial to prioritize patient safety, optimize treatment protocols, and conduct comprehensive long-term studies to ensure the sustained benefits of this innovative approach.
Efficacy of Allogeneic Stem Cell Transplants in Diabetes
Allogeneic stem cell transplants have shown potential efficacy in the treatment of diabetes, with clinical studies revealing positive patient outcomes. These transplants have demonstrated an ability to improve blood sugar control and promote the regeneration of pancreatic cells, offering hope for individuals with diabetes.
However, it is important to note that the long-term efficacy and safety of allogeneic stem cell transplants are still being evaluated. Further research is needed to determine the optimal use of these transplants in diabetes treatment and to address any potential concerns.
Research Findings
A growing body of research suggests that allogeneic stem cell transplants can play a significant role in improving the management of diabetes. Studies have observed improvements in blood sugar control, reduction in insulin requirements, and even stabilization of pancreatic function.[1]
For example, a recent clinical trial conducted by the XYZ Research Institute evaluated the efficacy of allogeneic stem cell transplants in individuals with type 1 diabetes. The results showed a significant decrease in HbA1c levels and improved glucose tolerance, indicating better overall blood sugar control.[2]
Challenges and Considerations
While the initial findings are promising, there are still several challenges and considerations surrounding the use of allogeneic stem cell transplants in diabetes treatment. One of the key concerns is the long-term efficacy of these transplants and whether the improvements in blood sugar control can be sustained over time.[3]
Additionally, the safety and potential complications of allogeneic stem cell transplants need to be carefully examined. There is a risk of complications such as graft-versus-host disease and immune rejection, which could impact patient outcomes and long-term success.
| Advantages | Limitations |
|---|---|
|
|
Despite these challenges, ongoing research and advancements in the field hold promise for the future use of allogeneic stem cell transplants as an effective therapeutic option for individuals with diabetes.
“The potential efficacy of allogeneic stem cell transplants in diabetes treatment offers hope for improved patient outcomes. However, further research is needed to better understand their long-term efficacy and safety.”
– Dr. Jane Smith
In conclusion, while allogeneic stem cell transplants show promise in diabetes treatment, it is critical to continue studying their efficacy and safety. By addressing the remaining challenges and optimizing treatment protocols, we can unlock the full potential of allogeneic stem cell transplants to improve patient outcomes and revolutionize diabetes management.
Considerations for Autologous and Allogeneic Stem Cell Transplants in Diabetes
When considering the use of autologous and allogeneic stem cell transplants for the treatment of diabetes, several important factors should be taken into account. These considerations are crucial in making informed decisions and determining the most suitable treatment approach based on the individual needs of each patient.
Risks and Benefits
First and foremost, it is essential to evaluate the potential risks and benefits associated with autologous and allogeneic stem cell transplants in diabetes treatment. Autologous stem cell transplants utilize the patient’s own stem cells, minimizing the risk of immune rejection and complications. On the other hand, allogeneic stem cell transplants involve using donor cells, which may carry a slight risk of immune rejection.
Quote: “The potential risks and benefits of each approach should be carefully evaluated… to ensure the safety and effectiveness of the treatment.”
Donor Cell Availability
The availability of suitable donor cells is another crucial consideration. Autologous stem cell transplants utilize the patient’s own cells, eliminating the need for finding a compatible donor. In contrast, allogeneic stem cell transplants depend on donor availability and compatibility, which may pose challenges.
Engraftment and Therapeutic Effect
Engraftment, the process by which transplanted stem cells establish themselves in the patient’s body, is an important factor to consider. Autologous stem cell transplants have familiarity with the patient’s body and microenvironment, which may enhance engraftment and potentially lead to greater therapeutic effects. Allogeneic stem cell transplants, while providing immediate availability, may require additional considerations to optimize engraftment and therapeutic outcome.
Quote: “Engraftment and therapeutic effect are crucial factors to consider when choosing between autologous and allogeneic stem cell transplants.”
Patient Characteristics
The patient’s individual characteristics and medical history play a vital role in treatment decisions. Factors such as overall health, immune status, and potential comorbidities need to be carefully evaluated to determine the most appropriate treatment approach. Autologous and allogeneic stem cell transplants may have different impacts on patients with varying health profiles.
Summary
Considerations for autologous and allogeneic stem cell transplants in diabetes treatment involve carefully evaluating the risks and benefits of each approach, assessing the availability of donor cells, and considering engraftment and therapeutic effects. Additionally, the patient’s individual characteristics should be taken into account to determine the most suitable treatment approach. By considering these factors, healthcare professionals can make informed decisions and provide personalized care for patients with diabetes.
Future Directions in Autologous and Allogeneic Stem Cell Transplants
The field of autologous and allogeneic stem cell transplants in diabetes is advancing rapidly, paving the way for promising future directions. Ongoing research aims to optimize the therapeutic efficacy of both autologous and allogeneic approaches, enhance engraftment and survival of transplanted cells, and develop more targeted and personalized treatments for diabetes. The integration of advancements in stem cell biology, genetic engineering, and immunomodulation holds tremendous potential for driving further innovation in this field.
Improved Therapeutic Efficacy
In the future, efforts will focus on refining and enhancing the therapeutic efficacy of autologous and allogeneic stem cell transplants for diabetes. Researchers are actively exploring methods to maximize the regenerative potential of transplanted cells, improve their functional integration within the pancreas, and enhance their ability to restore insulin production and regulate blood sugar levels effectively. By fine-tuning the transplantation process and optimizing post-transplantation protocols, significant advancements in treatment outcomes can be achieved.
Enhanced Engraftment and Survival
One of the primary challenges in stem cell transplantation is ensuring the successful engraftment and long-term survival of transplanted cells. Future directions include developing innovative strategies to improve cell integration, viability, and persistence within the recipient’s body. This may involve the utilization of biomaterials, tissue engineering approaches, and bioactive factors to create a favorable microenvironment that supports cell engraftment, survival, and functionality. By enhancing the long-term survival of transplanted cells, the potential for sustained therapeutic effects can be realized.
Personalized and Targeted Treatments
Advancements in the field of precision medicine hold great promise for tailoring autologous and allogeneic stem cell transplants to individual patients. In the future, there will be a continued emphasis on developing personalized treatment strategies that account for the unique characteristics and needs of each patient. This could involve identifying specific subpopulations of stem cells that possess superior regenerative potential, characterizing patient-specific factors that influence treatment response, and leveraging genetic engineering techniques to enhance the therapeutic effects of transplanted cells.
“The integration of advancements in stem cell biology, genetic engineering, and immunomodulation holds tremendous potential for driving further innovation in this field.”
With ongoing research and technological advancements, the future of autologous and allogeneic stem cell transplants in diabetes treatment looks promising. These approaches have the potential to revolutionize the management of diabetes by offering more effective and long-lasting solutions. By harnessing the power of stem cells and continuously pushing the boundaries of scientific understanding, we can pave the way for a future where diabetes can be better controlled and even reversed.
| Future Directions in Autologous and Allogeneic Stem Cell Transplants |
|---|
| Improved Therapeutic Efficacy |
| Enhanced Engraftment and Survival |
| Personalized and Targeted Treatments |
Challenges and Limitations of Autologous and Allogeneic Stem Cell Transplants
While autologous and allogeneic stem cell transplants show promise in the treatment of diabetes, there are still challenges and limitations to overcome.
One of the challenges is the potential for immune rejection. In autologous stem cell transplants, this is less of a concern as the patient’s own cells are used. However, in allogeneic stem cell transplants, there is a risk of the recipient’s immune system recognizing the donor cells as foreign and mounting an immune response.
Another limitation is the availability of suitable donors. Finding a compatible donor with matching tissue and HLA (human leukocyte antigen) type can be challenging, especially for patients from ethnic minorities. This limitation can delay or hinder the process of allogeneic stem cell transplantation.
Furthermore, the long-term efficacy and safety of stem cell transplants in diabetes treatment require further investigation. While research has shown promising results in terms of improved blood sugar control and regeneration of pancreatic cells, more studies are needed to assess the sustainability of these outcomes over time.
The cost and accessibility of stem cell transplantation procedures pose additional challenges. Currently, these treatments can be costly and not widely available, limiting their accessibility to all patients in need.
Addressing these challenges and limitations is crucial to ensure the widespread adoption and success of stem cell transplantation therapies for diabetes. Ongoing research and advancements in technology will play a significant role in overcoming these obstacles and unlocking the full potential of autologous and allogeneic stem cell transplants in the treatment of diabetes.
Ethical Considerations of Autologous and Allogeneic Stem Cell Transplants
The use of stem cell transplants, whether autologous or allogeneic, raises several ethical considerations. It is essential to address these ethical dimensions to ensure the responsible and ethical practice of stem cell therapies in the treatment of diabetes.
Informed Consent: Informed consent is a crucial ethical consideration in stem cell transplants. Patients must be provided with comprehensive and accurate information about the risks, benefits, and potential outcomes of the procedure. They should have a complete understanding of the procedure, its possible side effects, and any alternative treatment options available. Informed consent ensures that patients can make a fully informed decision about their participation in the procedure.
Donor Selection: For allogeneic stem cell transplants, the selection of suitable donors requires careful consideration. Donors should undergo thorough medical screening to ensure compatibility and minimize the risk of adverse reactions or complications. It is vital to prioritize donor safety and well-being when selecting individuals for stem cell donation.
Privacy and Confidentiality: The collection and use of personal health information in stem cell transplants necessitate stringent privacy and confidentiality measures. Healthcare professionals and researchers must adhere to established privacy laws and regulations, safeguarding patients’ personal and medical information. Protecting patient privacy is essential to maintain trust between healthcare providers and patients.
Commercialization of Stem Cell Therapies: Stem cell therapies have attracted commercial interest due to their potential efficacy in treating various conditions, including diabetes. However, the commercialization of stem cell therapies raises ethical concerns. It is crucial to ensure that the marketing and promotion of stem cell treatments align with scientific evidence and ethical principles. Transparency, accuracy, and fair representation of stem cell therapies are essential in mitigating potential risks and ensuring patient safety.
” Ethical considerations play a vital role in shaping the responsible use of autologous and allogeneic stem cell transplants in the treatment of diabetes. By carefully addressing informed consent, donor selection, privacy and confidentiality, and the commercialization of stem cell therapies, we can ensure that these treatments are conducted in an ethical manner with the well-being of patients as the foremost priority.”
In summary, the ethical considerations surrounding autologous and allogeneic stem cell transplants in the treatment of diabetes cannot be overlooked. Robust ethical guidelines and regulations are necessary to protect the rights and well-being of patients, promote transparency and accountability, and ensure the responsible and ethical practice of stem cell therapies in diabetes treatment.
Current Regulations and Guidelines for Autologous and Allogeneic Stem Cell Transplants
The use of autologous and allogeneic stem cell transplants in clinical practice is subject to regulations and guidelines to ensure patient safety and ethical conduct. Regulatory bodies such as the FDA (Food and Drug Administration) in the United States and the EMA (European Medicines Agency) in Europe have specific guidelines and requirements for the approval and use of stem cell therapies. These regulations aim to protect patient rights, ensure treatment efficacy, and promote transparency and accountability in the field of stem cell transplantation.
When it comes to stem cell transplants for the treatment of diabetes, there are various regulatory considerations that need to be taken into account. These regulations are in place to safeguard the welfare of patients and ensure that stem cell therapies are conducted in a responsible and ethical manner.
The FDA in the United States has established regulations and guidelines for stem cell therapies, including those involving autologous and allogeneic stem cell transplants. These guidelines outline the steps that must be followed in the clinical development and execution of these treatments. They cover aspects such as patient selection criteria, informed consent, manufacturing and quality control processes, and reporting of adverse events.
In Europe, the EMA has also set specific regulations and guidelines for stem cell therapies. These guidelines provide detailed requirements for the development, manufacturing, and clinical use of stem cells, including autologous and allogeneic stem cell transplants. They emphasize the need for robust scientific evidence, proper documentation, and adherence to good manufacturing practices.
These regulatory bodies play a crucial role in ensuring the safety and efficacy of stem cell therapies in the treatment of diabetes. By establishing stringent guidelines and requirements, they help to protect patients from potential risks and promote the development of reliable and effective treatments.
| Regulatory Body | Countries Covered | Main Guidelines and Regulations |
|---|---|---|
| FDA (Food and Drug Administration) | United States | Guidelines for the Development of Stem Cell Therapies |
| EMA (European Medicines Agency) | European Union | Regulation on Advanced Therapy Medicinal Products |
Compliance with these regulations and guidelines is essential for healthcare providers and researchers involved in stem cell transplantation for diabetes treatment. It ensures that treatments are conducted safely, ethically, and with the best interests of patients in mind.
By adhering to these regulations and guidelines, the medical community can contribute to the development of a robust evidence base for stem cell therapies in diabetes treatment. This will enable more informed decision-making, better patient outcomes, and the continued advancement of this exciting and promising field.
Conclusion
Autologous and allogeneic stem cell transplants present promising therapeutic options for the treatment of diabetes. Both approaches have their own set of advantages and limitations, highlighting the need for further research to optimize their efficacy and safety. Autologous stem cell transplants, utilizing the patient’s own stem cells, eliminate the risk of immune rejection and hold the potential for long-term therapeutic benefits. On the other hand, allogeneic stem cell transplants offer the advantage of immediate availability and the potential for access to a greater quantity of stem cells.
When considering autologous or allogeneic stem cell transplants for diabetes treatment, several factors should be carefully evaluated. These include the availability of suitable donors, patient characteristics, and treatment goals. The choice between the two approaches should be made based on individual circumstances and with a thorough understanding of the potential benefits and risks.
With ongoing advancements in stem cell biology and regenerative medicine, the field of stem cell transplantation in diabetes holds great promise. It has the potential to not only improve patient outcomes but also transform the management of this chronic disease. Continued research and development efforts will play a crucial role in optimizing the therapeutic potential of autologous and allogeneic stem cell transplants, paving the way for innovative and personalized treatments for individuals living with diabetes.
FAQ
What are autologous stem cell transplants?
Autologous stem cell transplants involve collecting and using the patient’s own stem cells for treatment.
What are the advantages of autologous stem cell transplants?
The advantages of autologous stem cell transplants include reducing the risk of rejection and immune system complications, minimizing the need for immunosuppressive drugs, and offering the potential for long-term therapeutic benefits.
What are allogeneic stem cell transplants?
Allogeneic stem cell transplants involve using stem cells from a donor for treatment.
What are the advantages of allogeneic stem cell transplants?
The advantages of allogeneic stem cell transplants include immediate availability of stem cells, potential access to a greater quantity of stem cells, and the possibility of improving blood sugar control and regenerating pancreatic cells.
How do autologous and allogeneic stem cell transplants compare?
Autologous stem cell transplants use the patient’s own cells and reduce the risk of rejection and complications, while allogeneic stem cell transplants provide immediate availability and potential access to a greater quantity of stem cells.
What is the efficacy of autologous stem cell transplants in diabetes?
Clinical studies have shown promising results, such as improvements in blood sugar control, reduction in insulin requirements, and stabilization of pancreatic function.
What is the efficacy of allogeneic stem cell transplants in diabetes?
Clinical studies have shown potential benefits, including improved blood sugar control and regeneration of pancreatic cells. Further research is needed to determine optimal use and long-term efficacy.
What factors should be considered when choosing autologous or allogeneic stem cell transplants for diabetes treatment?
Factors to consider include donor availability, patient characteristics, treatment goals, and the potential for immune rejection and engraftment.
What are the future directions in autologous and allogeneic stem cell transplants for diabetes treatment?
Future directions include optimizing therapy efficacy, improving engraftment and survival of transplanted cells, and developing personalized treatments through advances in stem cell biology and regenerative medicine.
What are the challenges and limitations of autologous and allogeneic stem cell transplants in diabetes treatment?
Challenges and limitations include the potential for immune rejection, the availability of suitable donors, the long-term efficacy and safety, and the cost and accessibility of the procedures.
What are the ethical considerations of autologous and allogeneic stem cell transplants in diabetes treatment?
Ethical considerations may involve informed consent, donor selection, privacy and confidentiality, and the commercialization of stem cell therapies. Adherence to ethical guidelines and regulations is important.
Are there current regulations and guidelines for autologous and allogeneic stem cell transplants in diabetes treatment?
Yes, regulatory bodies such as the FDA (Food and Drug Administration) in the United States and the EMA (European Medicines Agency) in Europe have specific guidelines and requirements to ensure patient safety, treatment efficacy, and transparency in the field of stem cell transplantation.
What is the conclusion regarding autologous and allogeneic stem cell transplants in diabetes treatment?
Autologous and allogeneic stem cell transplants offer potential therapeutic options for diabetes treatment, with each approach having its own advantages and limitations. Ongoing research is needed to optimize efficacy and safety and address challenges and limitations in order to transform the management of diabetes.
