Welcome to our deep dive into the world of stem cell transplants, particularly focusing on autologous and allogeneic transplants in the treatment of autoimmune diseases. If you’re exploring options for stem cell therapy, or simply want to understand more about this cutting-edge area of medicine, you’ve come to the right place. We’ll navigate through the complex but fascinating terrain of stem cell transplants, explaining everything in a way that’s informative yet easy to grasp.
What are Stem Cell Transplants?
Imagine your body as a complex city, and stem cells as the versatile construction workers capable of rebuilding damaged or diseased parts. In a stem cell transplant, these ‘construction workers’ are transferred from one part of the body to another, or from one person to another, to repair or replace damaged tissues. It’s like a renovation project for your body, where the goal is to fix the underlying issues causing disease.
The Battle Against Autoimmune Diseases
In autoimmune diseases, the body’s immune system, which typically guards against invaders like bacteria and viruses, mistakenly attacks its own tissues. It’s like having a security system that turns against the very home it’s meant to protect. Stem cell transplants offer a way to reset this misfiring immune system.
The Focus of Our Article
In this article, we’ll explore two primary types of stem cell transplants used in treating autoimmune diseases:
- Autologous Stem Cell Transplants: Here, the patient’s own stem cells are used. Think of it as using your own bricks and mortar for the repair work.
- Allogeneic Stem Cell Transplants: This involves stem cells donated by another person, introducing new building materials into the patient’s body.
We’ll compare and contrast these two approaches, delving into their procedures, benefits, risks, and how they fare against each other in treating various autoimmune conditions. Whether you’re a patient, a caregiver, or just someone interested in this field, our goal is to provide you with a comprehensive understanding of these transformative therapies.
Stay tuned as we embark on this journey to unravel the complexities of autologous and allogeneic stem cell transplants in the battle against autoimmune diseases.
Understanding Stem Cell Transplants
Definition and Types of Stem Cells
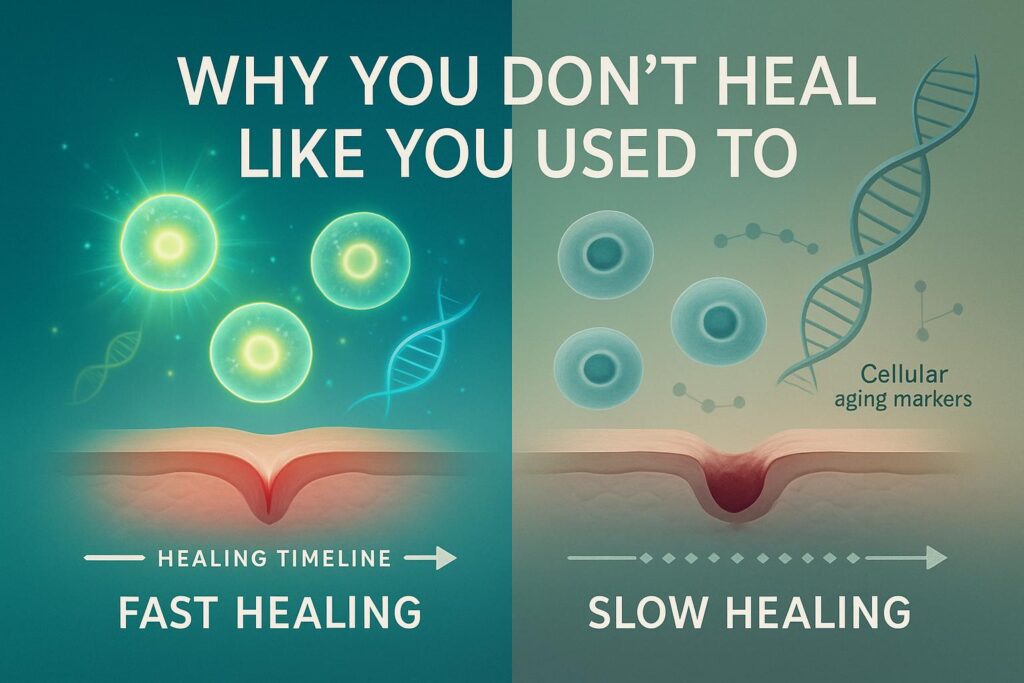
To truly appreciate the power of stem cell transplants, it’s crucial to first understand what stem cells are. Picture stem cells as the body’s raw materials, the cells from which all other cells with specialized functions are generated. They can be broadly classified into two types:
- Embryonic Stem Cells: These are like the master keys, capable of turning into any type of cell in the body.
- Adult Stem Cells: More specialized than embryonic stem cells, they’re found in various tissues and help in repairing and maintaining the body.
Autologous Stem Cell Transplants
Procedure
In an autologous stem cell transplant, the patient’s own stem cells are harvested, usually from the bone marrow or peripheral blood. After undergoing a treatment that eradicates diseased cells (often high-dose chemotherapy), these harvested cells are returned to the patient’s body, kickstarting the regeneration process.
Advantages
- Reduced Risk of Rejection: Since the stem cells come from the patient, the body is less likely to reject them.
- No Donor Required: Eliminates the need for a compatible donor, which can often be a hurdle in transplant procedures.
Limitations
- Potential for Disease Recurrence: As the cells are from the patient, they might carry the same genetic defects that caused the disease.
Allogeneic Stem Cell Transplants
Procedure
In contrast, allogeneic stem cell transplants involve stem cells donated by another person. This requires a matching process to ensure the donor’s cells are as compatible as possible with the recipient’s immune system.
Advantages
- Potential for a More Complete Disease Eradication: The donor’s healthy cells can completely replace the recipient’s faulty immune system.
- Graft-versus-Disease Effect: Donor cells might attack any remaining diseased cells, offering additional therapeutic benefits.
Limitations
- Risk of Graft-versus-Host Disease (GVHD): The donor’s immune cells might attack the recipient’s body, leading to complications.
- Dependency on Donors: Finding a compatible donor can be challenging.
| Type of Transplant | Source of Stem Cells | Advantages | Limitations |
|---|---|---|---|
| Autologous | Patient’s own body | Reduced rejection risk, no donor needed | Potential for disease recurrence |
| Allogeneic | Donor | More complete disease eradication, beneficial graft-versus-disease effect | Risk of GVHD, dependency on donors |
Both autologous and allogeneic transplants have their unique strengths and challenges. The choice between them depends on various factors, including the type of autoimmune disease, the patient’s overall health, and the availability of donors. Next, we’ll delve deeper into how these two approaches compare in treating autoimmune diseases.
Comparative Analysis: Autologous vs Allogeneic
When it comes to treating autoimmune diseases with stem cell transplants, choosing between autologous and allogeneic options is like deciding between two distinct paths, each with its own set of benefits and challenges. Let’s compare them across various parameters:
Efficacy in Treating Autoimmune Disorders
- Autologous: Often preferred for certain autoimmune diseases like multiple sclerosis (MS), where the goal is to reset the immune system. Studies show significant improvements in disease progression and symptom management.
- Allogeneic: More effective in cases where a complete immune system overhaul is necessary. It’s like rebooting a computer to get rid of a persistent virus. However, it’s used less frequently due to higher risks.
Risk and Complication Profiles
- Autologous: Lower risk profile, primarily because of the reduced chance of GVHD. It’s akin to renovating your house with your own tools and materials – familiar and generally safer.
- Allogeneic: Carries a higher risk, especially due to GVHD. It’s like bringing in external contractors for renovation; they might do a great job, but there’s also a risk they won’t align with the existing structure.
Patient Suitability and Selection Criteria
- Autologous: Suitable for patients who have a relatively well-functioning bone marrow and can tolerate high-dose chemotherapy.
- Allogeneic: Ideal for younger patients with more aggressive autoimmune diseases, where a radical approach is needed.
Long-term Outcomes and Quality of Life
- Autologous: Shows promising long-term remission in diseases like MS, with improved quality of life.
- Allogeneic: Can lead to long-term disease control, but the journey might be more complicated due to the potential for serious complications.
| Comparison Factor | Autologous Transplant | Allogeneic Transplant |
|---|---|---|
| Efficacy | High in specific diseases like MS | More comprehensive immune reset |
| Risk Profile | Lower (reduced GVHD risk) | Higher (increased GVHD risk) |
| Patient Suitability | Well-functioning marrow, can tolerate chemotherapy | Younger, more aggressive disease |
| Long-term Outcomes | Promising remission, improved quality of life | Long-term control, but with potential complications |
In summary, the choice between autologous and allogeneic stem cell transplants for autoimmune diseases is not one-size-fits-all. It’s a decision best made by weighing the individual’s specific condition, the severity of the disease, and the potential risks and benefits of each approach. Next, we will explore some real-world case studies and clinical trials to further understand the impact of these treatments.
Case Studies and Clinical Trials
Diving into case studies and clinical trials gives us a real-world glimpse into the outcomes and advancements in stem cell transplants for autoimmune diseases. These studies are like detailed maps that guide us through the terrain of medical science, showing us what works, what doesn’t, and where we can improve.
Review of Key Studies
- Multiple Sclerosis (MS): Numerous studies have highlighted the effectiveness of autologous hematopoietic stem cell transplantation (HSCT) in halting disease progression in MS patients, particularly those not responding to standard therapies.
- Systemic Sclerosis: Trials have demonstrated significant improvements in survival rates and symptom reduction following autologous HSCT.
Patient Outcomes and Experiences
The stories of patients who’ve undergone these transplants are compelling. Many MS patients treated with autologous HSCT have experienced periods of remission, some even returning to daily activities they couldn’t perform before the transplant. However, it’s crucial to remember that each patient’s journey is unique.
Emerging Trends in Research
Current research is exploring:
- Refining Patient Selection: Identifying which patients are most likely to benefit from either autologous or allogeneic transplants.
- Improving Safety: Developing protocols to reduce risks, especially in allogeneic transplants.
- Expanding Applications: Investigating the effectiveness of stem cell transplants in other autoimmune diseases.
| Disease | Transplant Type | Key Findings |
|---|---|---|
| MS | Autologous HSCT | Halted disease progression in many cases |
| Systemic Sclerosis | Autologous HSCT | Improved survival rates and symptom reduction |
The landscape of stem cell transplants in treating autoimmune diseases is ever-evolving, driven by ongoing research and patient experiences. As we continue to gather more data and insights, these treatments become more refined and effective.
Next, let’s hear from the experts in the field and look at the current guidelines and recommendations shaping the use of stem cell transplants in autoimmune diseases.
Expert Opinions and Consensus
Gleaning insights from experts and understanding the consensus within the medical community adds depth to our understanding of stem cell transplants in autoimmune disorders. These perspectives are like the compass guiding the ship of medical practice and research.
Current Guidelines and Recommendations
Organizations like the European Society for Blood and Marrow Transplantation (EBMT) and the American Society for Transplantation and Cellular Therapy (ASTCT) have set forth guidelines that stress:
- Patient Selection: Emphasizing the importance of choosing the right candidates for each type of transplant.
- Post-Transplant Care: Outlining the need for comprehensive follow-up care to manage complications and assess long-term outcomes.
Future Directions in Stem Cell Therapy for Autoimmune Disorders
The field is moving towards:
- Personalized Approaches: Tailoring treatments to individual patient profiles for maximum effectiveness.
- Integrating New Technologies: Utilizing advancements like gene editing to enhance the safety and efficacy of transplants.
Expert opinions and current guidelines form a crucial part of the decision-making process in stem cell transplantation for autoimmune diseases. They provide a framework that helps healthcare providers and patients navigate the complex choices in treatment options.
Next, we will explore the patient considerations – the decision-making process, cost, and accessibility issues, and support systems available for those considering stem cell transplants.
Patient Considerations
For patients considering stem cell transplants for autoimmune diseases, there are several key factors to weigh. This journey is not just about medical procedures; it’s about understanding the implications, making informed decisions, and navigating the path ahead with the right support.
Decision-making Process for Patients
The decision to undergo a stem cell transplant involves a thorough evaluation of:
- Disease Severity: How aggressive or advanced is the autoimmune disease?
- Individual Health: Is the patient’s overall health condition suitable for a transplant?
- Potential Risks and Benefits: Balancing the efficacy of the procedure against possible complications.
It’s a bit like deciding whether to undertake a major home renovation – you need to assess the condition of the house, the potential benefits of the renovation, and the risks or disruptions it may involve.
Cost and Accessibility Issues
The financial aspect of stem cell transplants cannot be overlooked. Patients need to consider:
- Insurance Coverage: Understanding what portions of the treatment are covered.
- Out-of-Pocket Expenses: Preparing for potential costs not covered by insurance.
- Access to Treatment Centers: Availability of specialized facilities and experts.
Support Systems and Resources
- Patient Support Groups: Connecting with others who have undergone similar procedures can be incredibly beneficial.
- Medical Team: Ongoing communication with healthcare providers is crucial for managing expectations and post-transplant care.
- Educational Resources: Utilizing materials provided by healthcare institutions and reputable online sources for additional information.
| Aspect | Considerations |
|---|---|
| Decision-making | Disease severity, individual health, risk-benefit analysis |
| Cost and Accessibility | Insurance, out-of-pocket expenses, access to centers |
| Support Systems | Patient groups, medical team, educational resources |
Navigating the world of stem cell transplants for autoimmune diseases is a journey that involves careful consideration, financial planning, and emotional support. It’s essential for patients to have access to all necessary information and support systems to make the best decision for their health and well-being.
Next, we will delve into the ethical and regulatory aspects surrounding stem cell transplants, exploring how these factors impact treatment availability and research progression.
Ethical and Regulatory Aspects
The realm of stem cell transplants, especially in the context of autoimmune diseases, is not just a scientific and medical frontier but also a domain deeply intertwined with ethical and regulatory considerations. These aspects are like the guardrails that ensure the safety, efficacy, and fairness of these advanced medical procedures.
Ethical Considerations in Stem Cell Research
- Informed Consent: Ensuring patients fully understand the risks, benefits, and alternatives to stem cell transplants.
- Use of Stem Cells: Ethical sourcing and use of stem cells, especially concerning embryonic stem cells.
- Equity in Access: Addressing disparities in access to these advanced treatments across different populations.
Regulatory Frameworks and Compliance
Globally, regulatory bodies like the FDA in the U.S., the EMA in Europe, and others set stringent standards for stem cell therapies. These regulations cover:
- Clinical Trial Approvals: Ensuring that trials are conducted ethically and safely.
- Therapy Approval Process: Rigorous review of treatments before they become widely available.
- Ongoing Monitoring: Post-market surveillance to track the long-term effects of these therapies.
Impact on Treatment Availability
The ethical and regulatory landscapes significantly influence the availability of stem cell treatments. While these regulations are crucial for patient safety, they can also slow down the process of bringing new therapies to the market. It’s a delicate balance between innovation and safeguarding public health.
| Aspect | Key Points |
|---|---|
| Ethical Considerations | Informed consent, ethical use of stem cells, equity in access |
| Regulatory Frameworks | Clinical trial and therapy approvals, ongoing monitoring |
| Treatment Availability | Balancing safety with the need for innovative treatments |
Navigating the ethical and regulatory aspects of stem cell transplants is crucial for ensuring these groundbreaking therapies are developed and applied responsibly and equitably. As we continue to push the boundaries of medical science, maintaining these standards is paramount for the benefit of patients and society at large.
Conclusion
In this exploration of autologous and allogeneic stem cell transplants for autoimmune diseases, we’ve traversed the landscape from the basic science behind these therapies to the real-world application, ethical considerations, and patient experiences. Each type of transplant offers unique advantages and comes with its own set of challenges, making the choice highly individualized.
The journey through the world of stem cell transplants is one of constant discovery and innovation. As research advances and clinical experiences accumulate, we edge closer to optimizing these therapies for those battling autoimmune diseases. The potential of stem cell transplants to significantly improve the quality of life for patients is immense, and with ongoing research, ethical considerations, and patient-focused approaches, the future of this field is bright and promising.
We hope this article has illuminated the complex yet fascinating world of stem cell transplants and provided valuable insights for those considering these treatments. The path to understanding and choosing the right treatment can be challenging, but with the right information and support, it becomes a journey of hope and possibility.